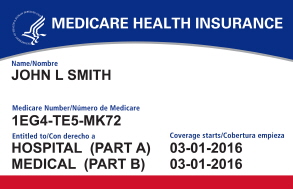
Hopefully, everyone that provides services to Medicare patients is aware of Medicare’s initiative regarding the replacement of Health Insurance Claim Numbers (HICNs). Basically, Medicare removed Social Security Number (SSN)-based Health Insurance Claim Numbers (HICNs) from Medicare cards and replaced those with Medicare Beneficiary Identifiers (MBIs). The MBIs will now be used for transactions like billing, eligibility status, and claim status.
In other words, every person with Medicare has been assigned an MBI and the HICN’s will not be used after December 31, 2019. Keep in mind that the MBIs are confidential and should be protected as Personally Identifiable Information.
Medicare did provide for a transition period and the same will end December 31st, 2019. As of January 1, 2020, all claims to Medicare should use the MBIs (regardless of date of service). Even after January 1st, 2020 there will be some exceptions such as:
- Appeals – People filing appeals can use either the HICN or the MBI for their appeals and related forms.
- Adjustments – HICN may be used indefinitely for some systems (Drug Data Processing, Risk Adjustment Processing, and Encounter Data) and for all records, not just adjustments.
- Reports – Medicare and some third-party Payors will continue to use HICN for a period of time.
- Reports to third-party Payors (quality reporting, Disproportionate Share Hospital data requests, etc.).
- Reports from Third-Party Payors (Provider Statistical & Reimbursement Report, Accountable Care Organization reports, etc.).
- Retrospective reporting – Plans can use the HICN when submitting data for older contract years for applicable systems (e.g., Health Plan Management System).
Fee-for-Service claim exceptions:
- Appeals – HICN or the MBI may be used for claims, appeals and related forms.
- Audits –HICN or the MBI may be used for audit purposes.
- Claim status query – The HICN or the MBI may be used to check the status of claims (276 transactions) if the earliest date of service on the claim is before January 1, 2020. MBI must be used for claims with a date of service on or after January 1, 2020.
- Span-date claims –HICN may be used for 11X-Inpatient Hospital, 32X-Home Health (home health claims & Request for Anticipated Payments (RAPs)), and 41X-Religious Non-Medical Health Care Institution claims if the “From Date” is before the end of the transition period (12/31/2019). Claims received between April 1, 2018 and December 31, 2019 may be submitted using either the HICN or the MBI. HICN or MBI may be used on claims in cases where patient started getting services in an inpatient hospital, home health, or religious non-medical health care institution before December 31, 2019, but stopped getting those services after December 31, 2019, even if billing was submitted after December 31, 2019.
- Incoming premium payments – People with Medicare who don’t get SSA or RRB benefits and submit premium payments should use the MBI on incoming premium remittances. But Medicare will accept the HICN on incoming premium remittances after the transition period. (Part A premiums, Part B premiums, Part D income related monthly adjustment amounts, etc.).
Our recommendations are as follows:
- Ask patients for their new Medicare cards. If they don’t have their cards, they have the option to call 1-800-MEDICARE (1-800-633-4227) or print them from gov.
- Obtain the MBI from Medicare or one of their intermediaries.
- Check your remittance advice for the MBI. The MBI is currently returned on the remittance advice for every claim submitted with a valid and active HICN through Dec. 31, 2019. Starting Jan. 1, 2020, claims will reject at the gateway. Therefore, you will no longer have the option for obtaining the MBI from the remittance advice.
- Verify your clearinghouse or vendor are submitting the MBI. If you use a clearinghouse or vendor to submit your Medicare claims, verify they are submitting with the MBI. If you send your claims to them with the MBI, but both the HICN and MBI are returned on your remittance advice, then they are not submitting your claims with the MBI.
