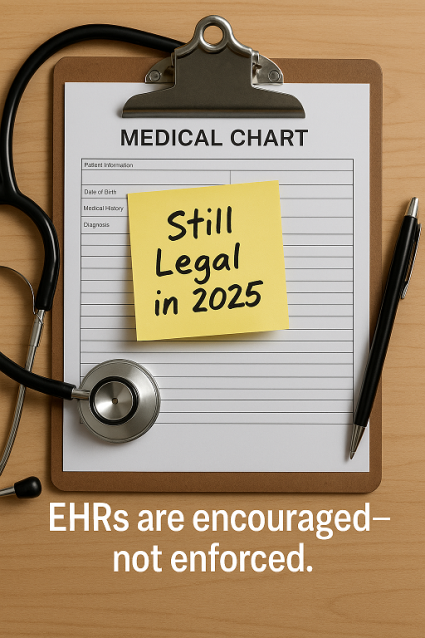
Why Electronic Health Records Aren’t Legally Mandatory—even in 2025
Many people still believe that Electronic Health Records (EHRs) are legally required across all healthcare settings. This misunderstanding is so common, we’ve named it “The EHR Myth.” While it’s true that the government heavily encourages the use of EHRs, no law demands their universal adoption. Instead, federal programs use financial carrots and sticks—but only for those who voluntarily opt in.
Reference: U.S. Department of Health and Human Services (HHS), Health IT Legislation Page
“The HITECH Act establishes programs under Medicare and Medicaid to provide incentive payments to eligible professionals… who adopt and meaningfully use certified EHR technology.”
Source: https://www.healthit.gov/topic/laws-regulation-and-policy/health-it-legislation
HITECH Encouraged EHRs, But Didn’t Require Them
The HITECH Act of 2009 revolutionized healthcare technology policy. It introduced significant funding and incentives for providers to adopt EHRs. However, HITECH never imposed a universal mandate. As the U.S. Department of Health and Human Services (HHS) states:
“Under the HITECH Act, eligible professionals who meet criteria may qualify for incentive payments.”
The catch? Only those who enrolled in these programs risk penalties for failing to meet EHR use benchmarks. According to HHS:
“Starting in 2015, hospitals and doctors will be subject to financial penalties under Medicare if they are not using electronic health records.”
That penalty applied only to participating providers—not to everyone. So The EHR Myth falls apart when we read the fine print.
Reference:
-
CMS HITECH Overview
“The Medicare and Medicaid EHR Incentive Programs… encourage eligible professionals to adopt, implement, upgrade, and demonstrate meaningful use of certified EHR technology.”
Source: https://www.cms.gov/regulations-and-guidance/legislation/ehrincentiveprograms -
Congressional Research Service (CRS) Report on HITECH
“HITECH… does not mandate adoption of health IT but encourages its use through financial incentives and penalties.”
Source: https://crsreports.congress.gov/product/pdf/R/R40161
Paper Records Are Still Legally Acceptable
Contrary to belief, providers who do not participate in federal EHR programs face no punishment for using paper records. The Centers for Medicare & Medicaid Services (CMS) continues to emphasize this voluntary structure:
“Medicare Promoting Interoperability Program participants may begin reporting and attesting their CY 2024 data in January 2025.”
In other words, if a provider doesn’t enroll, those rules—including penalties—don’t apply. This critical distinction is often misunderstood and adds fuel to The EHR Myth.
Reference:
-
CMS QPP 2024 Attestation Guidelines
“Participation in Promoting Interoperability is only required for MIPS eligible clinicians who choose to participate in the MIPS program.”
Source: https://qpp.cms.gov/mips/promoting-interoperability -
CMS on Promoting Interoperability Programs
“If a provider does not participate in the Medicare Promoting Interoperability Program, they are not subject to its requirements or penalties.”
Source: https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms
MACRA and MIPS: Payment Reform, Not Legal Mandate
In 2015, Congress passed MACRA, leading to the Merit-Based Incentive Payment System (MIPS). MIPS introduced performance-based payment adjustments—but only for eligible Medicare providers.
One of MIPS’s four performance categories is Promoting Interoperability, which evaluates EHR use. CMS describes requirements like:
“At least one permissible prescription … is transmitted electronically using certified electronic health record technology (CEHRT).”
“The MIPS eligible clinician … must attest they engage in bi-directional exchange … using CEHRT.”
However, MIPS participation is elective. Providers who don’t bill Medicare or opt out of MIPS are not obligated to report EHR activity. The EHR Myth collapses again under scrutiny.
Reference:
-
CMS QPP Overview
“MIPS is a voluntary program. Only MIPS-eligible clinicians are required to participate.”
Source: https://qpp.cms.gov/about/qpp-overview -
CMS Promoting Interoperability Performance Category
“To earn points in this category, MIPS eligible clinicians must use CEHRT and attest to performance.”
Source: https://qpp.cms.gov/mips/promoting-interoperability
Interoperability Is a Policy, Not a Law
Modern CMS rules aim to improve data exchange. For example, the 2020 Interoperability and Patient Access Final Rule promotes digital access and APIs. But even then, paper isn’t outlawed.
CMS says:
“This final rule is intended to move the health care ecosystem in the direction of interoperability … while minimizing reporting burdens.”
No regulation bans providers from using paper. So The EHR Myth continues to be more fiction than fact.
Reference:
-
CMS Interoperability and Patient Access Final Rule Fact Sheet
“The rule is designed to drive interoperability and patient access to health information… not to mandate EHR adoption.”
Source: https://www.cms.gov/newsroom/fact-sheets/interoperability-and-patient-access-fact-sheet
A Closer Look at the Original Misunderstanding
Some statements confuse HITECH’s purpose. For instance:
“The HITECH Act mandates the meaningful use of certified EHR technology … compliance is tied to Medicare and Medicaid incentive programs and penalties.”
That’s accurate—but only conditionally:
- ✅ Yes, HITECH mandates meaningful use for participating providers.
- ✅ Yes, non-compliance triggers penalties under Medicare.
- ❌ No, it doesn’t apply to every healthcare provider.
Again, The EHR Myth is based on misreading a policy choice as a legal mandate.
Reference:
-
HHS ONC HITECH Act Summary
“Meaningful use penalties only apply to eligible providers participating in the Medicare or Medicaid incentive programs.”
Source: https://www.healthit.gov/sites/default/files/hitech_act_excerpt_from_arra_with_index.pdf
Conclusion
To be clear: EHRs are not legally mandatory in the United States. Federal policy strongly supports them, but providers can still operate legally using paper. HITECH, MACRA, and MIPS offer incentives and attach conditions—but only when providers opt in.
In 2025 and beyond, the choice remains: EHRs are encouraged, but not enforced. Let’s stop assuming otherwise and finally bust The EHR Myth.
Reference:
-
GAO (Government Accountability Office) Report on EHR Incentives
“CMS does not require all providers to use EHRs. There are no enforcement actions or legal penalties for non-use outside the scope of its incentive programs.”
Source: https://www.gao.gov/products/gao-14-207 -
HHS FAQ (Office for Civil Rights)
“There is no federal requirement that medical records be electronic. Providers may still use paper records.”
Source: https://www.hhs.gov/hipaa/for-professionals/faq/medical-records
